 National HIV Curriculum Podcast
National HIV Curriculum Podcast
Disseminated MAC: Evaluation and Management


Transcript
Read along with the audio or jump to a particular chapter.
intro--case[00:00] Intro & Case
Hello everyone. I’m Dr. Jehan Budak from the University of Washington in Seattle and welcome to the National HIV Curriculum Podcast. This podcast is intended for health care professionals who are interested in learning more about the diagnosis, management, and prevention of HIV.
I’m back with my colleague, Aley Kalapila, an ID physician at Emory University in Atlanta. Hi Aley!
Dr. Kalapila
Hi Jehan. Hi everyone. Looking forward to this episode.
Dr. Budak
On today’s episode we’ll walk through a case of someone with advanced HIV and non-specific constitutional symptoms, a situation we often face. So, this patient is a 28-year-old man, who was very recently diagnosed with HIV and on the initial HIV clinic visit presented with fatigue and malaise. On exam, he was afebrile and had no focal findings. Baseline labs were obtained and he is immediately started on ART. One week later, he returns for a follow-up visit to review lab results and to check in. Lab work was notable for a CD4 count of 5 and a mild leukopenia of 3.2, mild anemia with hemoglobin/hematocrit 11/33, and a platelet count of 250. His comprehensive metabolic panel was normal. The baseline HIV RNA level was 150,000 [copies/mL]. So, Aley, what happened next?
1-week-follow-up[01:21] 1-Week Follow-up
Dr. Kalapila
When he came back to see me at this one-week follow-up visit after starting his antiretroviral therapy (ART), he still had some nonspecific fatigue and malaise, but overall, he was feeling better. I attributed a lot of that initial fatigue and malaise to the fact that he had advanced HIV. I also attributed the leukopenia and the anemia that he had to his advanced HIV as well. Since his CD4 count was less than 100, I had to obtain a screening serum cryptococcal antigen (or CrAg), as recommended by OI Guidelines for individuals with that CD4 count. That fortunately came back as negative. Because his CD4 count was less than 200, I started him on trimethoprim-sulfamethoxazole (or trim-sulfa) for PCP prophylaxis.
Dr. Budak
And so on the topic of prophylaxis, since his CD4 count was less than 50, did you consider prophylaxis against Mycobacterium avium complex, or MAC?
Dr. Kalapila
I did think about it, but the patient was started on antiretroviral therapy so, as per OI guidelines, I deferred the MAC prophylaxis.
Dr. Budak
For a little bit of background for the listeners, Mycobacterium avium complex is comprised of two different non-tuberculous mycobacteria, Mycobacterium avium and the other Mycobacterium intracellulare, that are ubiquitous in the environment. In persons without HIV, it typically causes pulmonary disease or lymphadenitis, the latter especially seen in children. On the other hand, in persons with HIV, it typically causes disseminated disease. In the past, the HHS OI, or Opportunistic Infections, guidelines used to recommend giving MAC prophylaxis for asymptomatic people with HIV who had a CD4 count less than 50. But this was updated a few years ago and now these guidelines state that primary MAC prophylaxis is not recommended if ART is initiated. And in this case, Aley, because you started him on ART, you did not give MAC prophylaxis. So, for the sake of discussion, what would you have done if this patient did not want ART?
Dr. Kalapila
Well, Jehan in that case, if the patient did not want to start antiretroviral therapy, then as per OI guidelines, he would need to initiate MAC prophylaxis. Before we do that, though, we would first need to rule out disseminated MAC disease, which can be done by doing two things. First, clinically, we have to look for signs and symptoms of disseminated MAC. So, this is usually a lot of constitutional symptoms that include fever, weight loss, night sweats, diarrhea, anemia, hepatosplenomegaly. The other thing that one would need to do is to actually obtain a baseline blood culture for acid-fast bacilli or AFB. Now, I do want to say that this situation, where someone doesn’t want to start ART, in general these days, quite rare. It’s unusual for people, especially if they are coming to clinic, to decline antiretroviral therapy but then agree to take MAC prophylaxis.
Dr. Budak
I totally agree. I think the last time I was in this scenario where someone didn’t want to take ART but was willing to take MAC prophylaxis was six years ago. So, it has been a while. But, back to this patient.
afb-blood-culture[04:37] AFB Blood Culture
Dr. Budak
He had a CD4 count less than 50 (his CD4 count was actually 5), he had vague constitutional symptoms, and some cytopenias. Did you get an AFB blood culture, even though you did not put him on MAC prophylaxis since he started ART?
Dr. Kalapila
Absolutely, yes. So, in this specific case, even though he started ART, as you mentioned, he did have these cytopenias, he had vague constitutional symptoms, which all could be representative of disseminated MAC or advanced HIV or both. And also, with that CD4 count less than 50, I did opt to obtain an AFB blood culture for this specific case.
Dr. Budak
Okay, so it sounds like you're getting AFB blood cultures for a diagnostic purpose, not for screening purposes. Cool. And this is actually a good time to pause and quickly review what the OI guidelines say about obtaining AFB blood cultures. They suggest that before primary prophylaxis is started, as Aley mentioned, disseminated MAC should be ruled out by a clinical assessment and if appropriate by obtaining an AFB blood culture. And this is to make sure that you're not giving a single antibiotic for prophylaxis when actually the patient has a cold infection requiring more than one antibiotic. Aley, to digress even a little bit more, if a patient does not want to take ART, and they're asymptomatic, would you have still gotten an AFB blood culture?
Dr. Kalapila
Usually yes. So, when patients have a CD4 count less than 50, and they're not planning to start ART, I do check an AFB blood culture regardless of their symptoms. This has been my practice primarily because it's a pretty easy lab to obtain, and oftentimes these patients, as we know, are very immunocompromised and as a result of sort of the severe immunocompromised may have very subtle clinical symptoms that they may just write off and attribute say to their HIV. So, in my mind, getting an AFB blood culture is a pretty easy thing to do that would definitively confirm if a patient has occult disseminated MAC.
Dr. Budak
I do the same. It's easy enough to get an AFB blood culture, and I do not see the harm doing so in situations when the patient is not planning on taking ART.
dmac-prophylaxis[06:37] dMAC Prophylaxis
Dr. Budak
If you were going to give MAC prophylaxis in this sort of hypothetical situation, what medication would you start?
Dr. Kalapila
So, the AFB blood cultures take about six weeks to finalize, right? They incubate it in the lab for six weeks, so we are not going to have a final result until six weeks. So, what I do is after I obtain the AFB blood cultures, I wait for about two weeks, and then I initiate MAC prophylaxis provided, at least up until that point, that the cultures have remained negative. And to start MAC prophylaxis, the drug that I use is azithromycin, and typically the dose that I use is 1200 milligrams once a week. Now for people that are unable to tolerate taking such a large dose at one time, I can split the dose up and give 600 milligrams two days per week. I, of course, am going to continue to follow those AFB blood cultures until six weeks out because they can turn positive later. And, of course, we know that the prolonged use of macrolides for MAC prophylaxis as monotherapy in a person with occult MAC infection can lead to macrolide resistance or antimicrobial resistance.
Dr. Budak
Aley, just to clarify for the learners, when you're talking about giving that option where you're doing 600 milligrams two times a week. I believe what Aley is referring to is 600 milligrams one day followed by 600 milligrams the next day, not 600 milligrams one day and then another 600 milligrams a couple of days later.
Dr. Kalapila
Yeah, exactly.
Dr. Budak
And again, to reiterate, if we are starting someone on ART with a CD4 count less than 50, then there is no need to start MAC prophylaxis, but if a person is not starting ART, then MAC prophylaxis should be initiated after evaluating for disseminated MAC. And after that digression, let me take us all back to the case.
So Aley, since you had started him on ART, you did not initiate MAC prophylaxis. When his CD4 resulted, you saw him back to discuss lab findings. That was one week later. You obtained a serum crag because his CD4 count was less than 100. Luckily that was negative. And you also obtained AFB blood cultures because although his fatigue and constitutional symptoms and cytopenias could have been due to untreated HIV, it could have also been due to disseminated MAC. Did I get that right?
Dr. Kalapila
Yeah, absolutely. I agree.
dmac-diagnosis[08:56] dMAC Diagnosis
Dr. Budak
And then after ART initiation, he seemed to be improving, but it sounds like three weeks into incubation of those AFB cultures, they grew MAC, what did you do then?
Dr. Kalapila
I asked him back to clinic, and fortunately he felt pretty good, and he was in good spirits after starting his ART. But, of course, I can't ignore that positive blood culture that is growing MAC, and so I started him on treatment for disseminated MAC or dMAC as we often refer to it.
Dr. Budak
So, before we talk about the specific antibiotics for treatment, let me expand on the diagnosis of dMAC. It is based on a compatible clinical syndrome combined with isolation of the organism, which we typically do by culture. The clinical syndrome, as Aley has intimated, is often nonspecific with constitutional symptoms. You may have exam findings that are notable for hepatosplenomegaly or diffuse lymphadenopathy. You may have lab abnormalities such as cytopenias and elevated LDH, which we know is a nonspecific marker of inflammation and can be elevated for many other reasons, and/or an elevated and oftentimes isolated alkaline phosphatase.
If you image a patient, you might see the findings of hepatosplenomegaly or sort of diffuse lymphadenopathy. And then for diagnosis, in addition to pairing that with the clinical syndrome, it's necessary to isolate the organism, which can be done either by obtaining blood cultures, which is the easiest to obtain as Aley did, or culture from a biopsy of a lymph node, bone marrow, or culture from another normally sterile site. So that was an aside.
dmac-tx[10:28] dMAC Tx
Dr. Budak
Let's go back to the MAC treatment. Aley, what did you give him?
Dr. Kalapila
I decided to treat him with azithromycin and ethambutol because he had reported clinical improvement, and so I opted not to give him rifabutin.
Dr. Budak
So, can you walk us through the basic principles of MAC treatment?
Dr. Kalapila
Absolutely. So much like other mycobacterial diseases, so for example, TB is the most common one we think about, tuberculosis, multi-drug therapy is the cornerstone of dMAC treatment. Now, the OI guidelines recommend that at least two drugs should be used as initial therapy for dMAC in order to avoid antimicrobial resistance. So, in many ways this is kind of similar in concept to TB, right? We start out with multiple drugs. Now the two drugs that are recommended for dMAC are macrolides, so that is either azithromycin or clarithromycin. And then the second drug is ethambutol.
Dr. Budak
And what's your preference on using azithromycin versus clarithromycin?
Dr. Kalapila
Great question. A lot of the literature that we have, the published data that we have, is with clarithromycin than with azithro but, in my clinical experience, what I found is that people have a lot more GI side effects with clarithromycin, and so I personally prefer to prescribe azithro because I find azithromycin to be much better tolerated. So, it is my go-to.
Dr. Budak
Totally agree with you. I also prefer azithromycin, and when I talk to learners about this, I mentioned the published data to which you referred and tell them that those are older papers and that I think nowadays most people feel comfortable with using azithromycin.
So back to the principles of dMAC treatment, you mentioned using at least two drugs, and you also mentioned that you had opted not to give him rifabutin. Can you talk a little bit more about times when you use more than two drugs?
Dr. Kalapila
I would consider adding a third drug if the patient has severe dMAC disease, or they're not on effective antiretroviral therapy. And by that, I mean if they are taking ART that doesn't result in adequate viral suppression or HIV RNA suppression. Now my biggest issue here is that the main third drug that we would all reach for is rifabutin because as we know, the rifamycin class of drugs, and rifabutin belongs to the rifamycin class, is notorious for drug-drug interactions, right? They're CYP450 inducers, and so you can get major drug interactions with antiretroviral therapy, and oftentimes we end up having to modify our antiretroviral therapy regimen if we're adding rifabutin to someone's dMAC treatment regimen.
severe-dmac-tx[13:10] Severe dMAC Tx
Dr. Budak
And you mentioned adding a third drug if the patient has severe dMAC. What constitutes severe disease? I know this is a bit subjective, so I'm curious what your clinical practice is.
Dr. Kalapila
I would consider the isolation of the organism from multiple sites as an indicator of severe DMAC. I would also go off the severity of the patient's symptoms. So now in those cases, I would balance the need to start this third drug, which is a rifamycin, along with the patient's willingness to actually take this because, as I just mentioned, we may very well need to modify the antiretroviral therapy regimen because of the drug-drug interactions.
Now the HHS OI guidelines reference the addition also of a fourth drug which may come into play if there was concern for drug resistance, which can occur with patients who don't initially tolerate their dMAC treatment and are maybe not taking their antimicrobial treatments consistently. So, in those cases, I would have to add on two additional drugs to get them adequate antimicrobial activity. The meds that are recommended in the OI guidelines for that fourth drug option would be fluoroquinolones, which are pretty well tolerated but comes with its own set of side effects, or an injectable aminoglycoside, which is much less tolerable.
Dr. Budak
Yeah, definitely much less tolerable, so hopefully can be avoided.
post-dmac-tx-initiation[14:32] Post dMAC Tx Initiation
Dr. Budak
Let's go back to the case, but fast-forward in the chronology. Your patient had been being managed as an outpatient and has been on dMAC treatment now for two to three weeks, and you had given him azithromycin and ethambutol when he actually developed new symptoms of abdominal cramping, night sweats, subjective fevers, shaking, chills, and inability to take anything by mouth due to nausea and vomiting. So, kind of like a recrudescence of things. He was trying to control his abdominal pain with acetaminophen and ibuprofen without improvement. And so, because of this, he came to the clinic for additional evaluation, and he states that he feels worse than he ever has. What did you do at this point?
Dr. Kalapila
Yeah, so I still always think about this case. He was looking extremely uncomfortable. He was writhing in pain on the bed in the office. I really was just unable to obtain a good abdominal exam because he was in so much discomfort. So, I actually ended up sending him to the emergency room for pain control and STAT imaging because there were so many things in my differential at that point in time. The most urgent of which would've been to rule out an acute abdominal process.
Dr. Budak
And I'll give some information from the ER/the admission. So, he did not have an acute abdominal process. His lab showed that his CD4 count had gone up to 19 from 5, that his HIV RNA was now undetectable, that his alk phos, or alkaline phosphatase, was in the thousands, and his AST and ALT were in the eighties, and they were all previously normal. A CT abdomen showed mild splenomegaly and diffuse abdominal lymphadenopathy with numerous retroperitoneal and mesenteric lymph nodes but a normal GI tract.
Dr. Kalapila
Yes. So based on these findings, the main thing that crossed my mind was MAC IRIS, or immune reconstitution inflammatory syndrome. Now given the degree of immunosuppression at the time of his HIV diagnosis, I didn't want to necessarily anchor on that diagnosis. I really thought this was going to be MAC IRIS, but I also had to consider the possibility that we had unmasked an additional occult infection or an occult AIDS associated malignancy.
Dr. Budak
An important thing to reiterate that we've done in multiple episodes is to remember that immunocompromised individuals can have more than one thing going on as Aley is thinking about. So how did you figure out what was going on with him?
Dr. Kalapila
Since the main findings on his CT showed diffuse abdominal lymphadenopathy, we discussed the case with an interventionist, and we obtained a biopsy of a retroperitoneal lymph node. Now we got pathology back, which showed granulomatous inflammation. So, with all of that data, I felt pretty comfortable giving him a diagnosis of MAC IRIS or IRIS to disseminated MAC, and I opted to treat him at that point with prednisone, and I started him on 40 milligrams once a day of prednisone.
mgmt-dmac-iris[17:24] Mgmt of dMAC IRIS
Dr. Budak
And Aley, a bit of a logistical question. I can imagine that there's a several day delay between biopsy and obtaining any result from pathology. So what's your approach to starting steroids empirically in that timeframe before we even have a definitive answer?
Dr. Kalapila
You're absolutely right that it does take some time to get those results back, and we're sort of sitting there trying to figure out what to do. And so because we had to rule out these other infections and malignancies, I kind of held off on initiating steroids, and I managed him with other supportive treatments that wouldn't necessarily impact the diagnosis or cause his symptoms to get worse. So, in this specific case, we ended up doing his pain control with opiates and anti-emetics while we were waiting for biopsy results to come back. Now, if the patient's symptoms had been extremely severe, then I would recommend initiating steroids empirically while obtaining that tissue for diagnosis. Now, there may also be circumstances that a tissue diagnosis may not be feasible to confirm, and if a situation like that arises, it would not be unreasonable to initiate corticosteroids again if you are unable to obtain tissue.
Dr. Budak
Yeah, it sounds like this is a gray zone and that if able to avoid steroids until a tissue diagnosis is established, that that is an ideal scenario. But sometimes empiric steroid initiation is necessary, and some clinicians in this particular case would've felt comfortable in giving him a presumptive diagnosis of dMAC IRIS and starting steroids even without pursuing biopsy. I think based on his labs, the new alk phos elevation, the mild transaminitis, his imaging findings with the diffuse lymphadenopathy, the mild splenomegaly, and his constitutional symptoms, along with the clinical history of recently initiated ART with rapid viral suppression and having a known recently positive AFB blood culture. So, all this to say gray zone. How did he do once you started him on the prednisone 40 milligrams daily?
Dr. Kalapila
Not surprisingly, he did incredibly well, as most patients do when they first get prednisone. So his symptoms markedly improved over the span of two to three weeks. He was completely back to normal. So, at the four-week point, I felt so great that I was like, I have to sort of in the long run get him off steroids because as we know, prolonged steroid use is not necessarily the best thing, plus it can also cause immunosuppression. So, I really was excited because he looked amazing, and I decided to do a rapid taper by dose reducing him about 10 milligrams weekly. But of course, few days into that, into his 30-milligram dose, he started to develop abdominal cramping, nausea, vomiting. He came back into clinic, and I was like, "Okay, this was too much." I was in too much of a rush, and I bumped him back up to 40. And eventually we did a prolonged and very slow taper over a course of several weeks.
when-to-start-art[20:11] When to Start ART
Dr. Budak
Thank you for sharing that because I think this is yet another gray zone where every patient and every IRIS is different and requires individualization and IRIS, which is actually is to a specific disease process that usually in the field of HIV can be either infectious or malignant, and so every IRIS is potentially to a different etiology, and every patient is different. So the treatment of IRIS, there's no one size fits all. And Aley, can you comment on ART management during this time and what you did with his dMAC therapy?
Dr. Kalapila
I continued his antiretroviral therapy throughout his IRIS because in the long run, he needs the immunity constitution in order to clear his MAC. And so this is why I opted to continue it. Now, it's really important to emphasize that although it might be tempting to stop the ART when you see someone suffering from MAC IRIS, it really has to be continued. As for his dMAC therapy, I continued it for at least 12 months, which is what is recommended in the HHS OI guidelines. And his CD4 needed to be at least a hundred for at least six months before I could discontinue the dMAC antibiotics. And I'm happy to report that he has done remarkably well - like one of my sort of success stories that I'm thrilled for - for this patient.
Dr. Budak
What a nice ending to this episode.
summary-points[21:34] Summary Points
Dr. Budak
So, let's wrap up with some summary points.
- MAC causes disseminated multi-organ infection in people with HIV, usually with a CD4 count less than 50.
- Primary prophylaxis against MAC is no longer routinely indicated if the person is started on fully suppressive ART.
- The diagnosis of MAC is based on isolating the organism from a sterile site, usually the blood, and preferred treatment is usually two-drug therapy, azithromycin plus ethambutol, and for at least one year though, there are some scenarios in which we may need to use a third drug.
- In general, ART can be started as soon as possible when someone has dMAC. And this is not a situation where you need to delay initiation of ART.
- MAC IRIS may occur, and symptoms can either be mild and self-limited or severe, requiring systemic corticosteroids for symptom management, and the patient should continue their ART while also receiving treatment for their MAC IRIS.
So, with that in mind, Aley, thank you so much. And until next time.
Dr. Kalapila
Bye, Jehan. Thanks.
credits[22:35] Credits
Transcripts and references for this podcast can be found on our website, the National HIV Curriculum at www.hiv.uw.edu. The production of this National HIV Curriculum Podcast was supported by Grant U10HA32104 from the Health Resources and Services Administration of the U.S. Department of Health and Human Services. Its contents are solely the responsibility of the University of Washington IDEA program and do not necessarily represent the official views of HRSA or HHS.
 Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy
Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza
Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Dolutegravir-Abacavir-Lamivudine Triumeq
Dolutegravir-Abacavir-Lamivudine Triumeq Dolutegravir-Lamivudine Dovato
Dolutegravir-Lamivudine Dovato Dolutegravir-Rilpivirine Juluca
Dolutegravir-Rilpivirine Juluca Doravirine-Tenofovir DF-Lamivudine Delstrigo
Doravirine-Tenofovir DF-Lamivudine Delstrigo Efavirenz-Tenofovir DF-Emtricitabine Atripla
Efavirenz-Tenofovir DF-Emtricitabine Atripla Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya
Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild
Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey
Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey Rilpivirine-Tenofovir DF-Emtricitabine Complera
Rilpivirine-Tenofovir DF-Emtricitabine Complera Enfuvirtide Fuzeon
Enfuvirtide Fuzeon Fostemsavir Rukobia
Fostemsavir Rukobia Ibalizumab Trogarzo
Ibalizumab Trogarzo Maraviroc Selzentry
Maraviroc Selzentry Dolutegravir Tivicay
Dolutegravir Tivicay Raltegravir Isentress
Raltegravir Isentress Abacavir Ziagen
Abacavir Ziagen Abacavir-Lamivudine Epzicom
Abacavir-Lamivudine Epzicom Abacavir-Lamivudine-Zidovudine Trizivir
Abacavir-Lamivudine-Zidovudine Trizivir Didanosine Videx
Didanosine Videx Emtricitabine Emtriva
Emtricitabine Emtriva Lamivudine Epivir
Lamivudine Epivir Stavudine Zerit
Stavudine Zerit Tenofovir alafenamide-Emtricitabine Descovy
Tenofovir alafenamide-Emtricitabine Descovy Tenofovir DF Viread
Tenofovir DF Viread Tenofovir DF-Emtricitabine Truvada and Multiple Generics
Tenofovir DF-Emtricitabine Truvada and Multiple Generics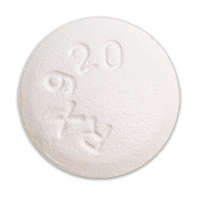 Zidovudine Retrovir
Zidovudine Retrovir Zidovudine-Lamivudine Combivir
Zidovudine-Lamivudine Combivir Doravirine Pifeltro
Doravirine Pifeltro Efavirenz Sustiva
Efavirenz Sustiva Etravirine Intelence
Etravirine Intelence Nevirapine Viramune
Nevirapine Viramune Rilpivirine Edurant
Rilpivirine Edurant Atazanavir Reyataz
Atazanavir Reyataz Atazanavir-Cobicistat Evotaz
Atazanavir-Cobicistat Evotaz Darunavir Prezista
Darunavir Prezista Darunavir-Cobicistat Prezcobix
Darunavir-Cobicistat Prezcobix Fosamprenavir Lexiva
Fosamprenavir Lexiva Indinavir Crixivan
Indinavir Crixivan Lopinavir-Ritonavir Kaletra
Lopinavir-Ritonavir Kaletra Nelfinavir Viracept
Nelfinavir Viracept Saquinavir Invirase
Saquinavir Invirase Tipranavir Aptivus
Tipranavir Aptivus Cobicistat Tybost
Cobicistat Tybost Ritonavir Norvir
Ritonavir Norvir